Takashi Kozai, Assistant Professor of Bioengineering at the University of Pittsburgh (Pitt) Swanson School of Engineering, has been awarded an R21 grant from the National Institutes of Health (NIH) to improve the design of chronic brain implants by investigating the role of oligodendrocytes and oligodendrocyte progenitor cells in the process of host tissue response.
Kozai will work with Franca Cambi, professor of neurology at Pitt, to develop in vivo imaging technology that will explore how these cells cause negative tissue response to chronic brain implants. Supported by the NIH’s National Institute of Neurological Disorders and Stroke, Kozai and Cambi received a two-year, $386,645 award for their research.
Oligodendrocytes and oligodendrocyte progenitor cells (OPCs) are a type of glia or connective tissue in the central nervous system that play an important role in brain injury and neuronal activity, including the body’s response to brain implants. Oligodendrocytes are crucial for normal signaling in the brain, producing proteins that help neurons grow and form synapses, and may even help neurons survive traumatic injuries. They play a key role in myelination, a process whereby oligodendrocytes wrap a fatty substance around the neuron’s axon to help insulate electrical signals and allow neural signals to move more rapidly.
“Oligodendrocytes, like neurons, consume enormous amounts of energy,” Kozai said. “Neurons require the energy to maintain membrane potential, while oligodendrocytes require energy to maintain high production levels of protein and lipids. As a result, oligodendrocytes and neurons are one of the first cell types to die following brain injury. Because the oligodendrocytes provide growth factors and support for neurons, the idea is maybe if we can help the oligodendrocytes to survive after injury, they can, in turn, help the neurons to survive.”
They plan to apply a similar logic to OPCs, which are a subtype of glia that are of particular interest because they have the capacity to differentiate into oligodendrocytes, astrocytes, or neurons during tissue repair.
“If we can maintain a healthy environment for OPCs, maybe they can help replenish the oligodendrocyte and neuronal population instead of turning into scar-tissue-forming astrocytes,” Kozai said.
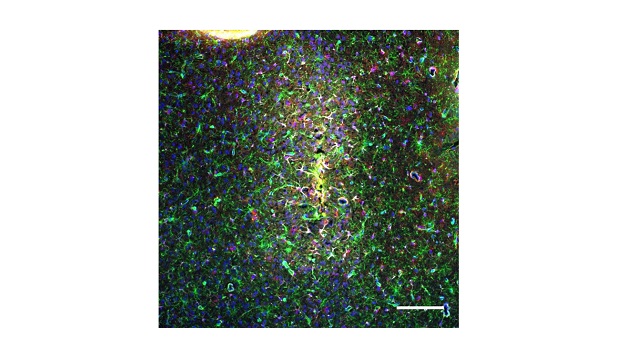
Kozai and Cambi hope to gain insight by getting a more detailed look at the life span of these cells using multiphoton imaging and neural engineering technology.
“Much of the work on oligodendrocytes and OPCs has been carried out with postmortem immunohistochemistry and molecular assays in disease models,” Kozai said. “As such, we only get a snapshot of the dead cells in their last moments, instead of seeing how and when they got there so that we can identify when and where to apply treatments and employ intervention strategies.”
By using in vivo imaging techniques like multiphoton imaging and pinpointing brain injury using neural engineering technology, Kozai and Cambi can map out the spatiotemporal relationships between oligodendrocyte loss, neuronal cell death, and OPC tissue repair and identify targets for intervention strategies, not just for brain implants but also for many neurodegenerative diseases.