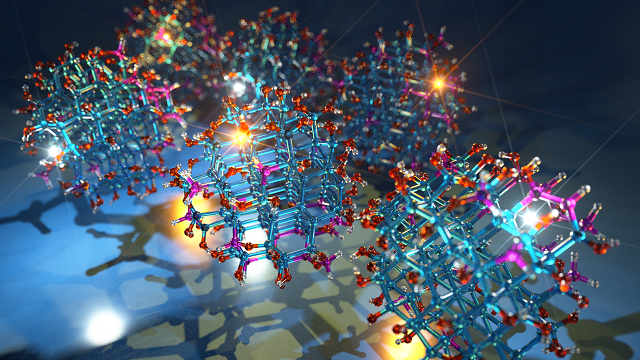
A novel proof-of-concept nanosystem for the visualization of tumors generates bright tumor signals by delivering near-infrared quantum dots (QDs) to cancer cells without any toxic effects. The QDs are delivered intravenously into extravascular tumor tissue and cells to gain bright tumor signals. Some QDs leave the bloodstream and cross membranes, entering cancer cells. Fluorescent signals emitted from excess QDs that remain in the bloodstream are made invisible by injecting a membrane-impermeable etchant to eliminate background signals.
The biocompatible QD platform loses photoluminescence upon cation exchange, which occurs when zinc in the QDs is exchanged for silver in the etchant. Silver-containing QDs lose their fluorescent capabilities, and because the etchant can’t cross membranes to reach tumor cells, the QDs that have reached the tumor remain fluorescent.
Subsequent etching quenches excess QDs, leaving a highly tumor-specific signal provided by the intact QDs remaining in the extravascular tumor cells and fibroblasts. Renal excretion of the cations released from the QDs minimizes potential toxicity.
“The novelty of our nanosystem is how the etchant works,” said researcher Gary Braun.
Researchers used a mice model harboring human breast, prostate and gastric tumors to develop the method. QDs were actively delivered to tumors using the iRGD peptide.
“To our knowledge, this is the first in vivo example of a background-destroying etchant being used to enhance the specificity of imaging,” said Kazuki Sugahara, M.D. “We are encouraged that we were able to achieve a tumor-specific contrast index (CI) between five- and ten-fold greater than the general cut-off for optical imaging, which is 2.5.”
The system also facilitates the detection of peritoneal tumors with high specificity upon intraperitoneal tumor targeting and selective etching of excess untargeted QDs.
“Moving forward we will focus on developing our novel nanosystem to work with routine imaging tests like PET scans and MRIs. In our studies with mice, we use optical imaging, which isn’t always practical for humans,” Sugahara said.
In vivo cation exchange could provide a way to enhance specificity of tumor imaging. A business is being formed to further develop the platform for human use.
The research was performed at Sandford-Burnham Prebys Medical Discovery Institute (SBP). The research was published in Nature Communications (doi:10.1038/s41467-017-00153-y).
Source: Photonicsmedia